Four million Americans suffer from glaucoma, an incurable eye disease that slowly degrades peripheral vision and eventually leads to blindness. Researchers at Georgia Tech have discovered a potential way to stop this degradation and possibly save people’s vision before it’s too late.
Raquel Lieberman, a professor in the School of Chemistry and Biochemistry and the Parker H. Petit Institute for Bioengineering and Bioscience, and her lab team have discovered two new antibodies with promise to treat glaucoma. The antibodies can break down the protein myocilin, which, when it malfunctions, can cause glaucoma.
Lieberman’s group recently published this research in the Proceedings of the National Academy of Sciences: Nexus.
Protein Problems
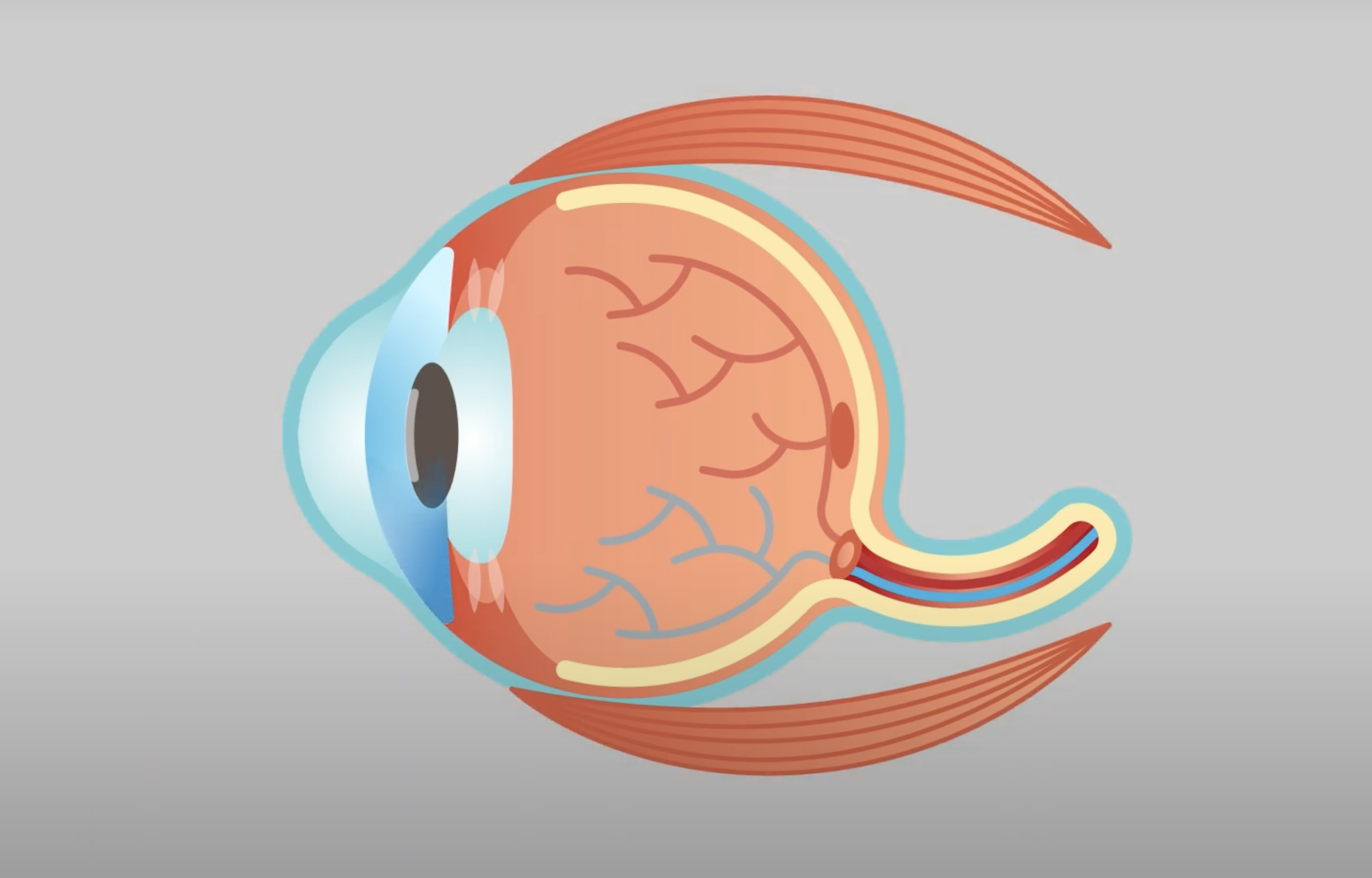
Myocilin is just one of hundreds of thousands of proteins that make up the human body. In the eye, an especially delicate balance of proteins and fluid enables sight. The aqueous humor, a clear fluid, bathes the lens that helps focus light into the retina. In a healthy eye, the fluid drains regularly, but if something prevents the fluid from circulating, it increases pressure.
“Your eyeball is kind of like a basketball,” explained Lieberman. “If you want it to work optimally, it has to be pressurized.”
Lieberman’s team has learned that if myocilin mutates, it clumps up and prevents aqueous humor from draining, increasing eye pressure. If left unmanaged, glaucoma and — eventually — blindness will occur.
Antibody Answer
Lieberman’s lab characterized two new antibodies that each, in their unique way, can destroy myocilin gone rogue. One binds in a way that does not prevent myocilin from clumping; the other prevents the protein from aggregating. Both effectively break down myocilin so it no longer blocks the aqueous humor from flowing.
“These exciting results provide proof of concept that targeted antibodies for mutant myocilin aggregation could be therapeutic,” said Alice Ma, a Ph.D. graduate who worked on the research. “This represents a new paradigm for treating other diseases associated with protein clumping, like Alzheimer’s. These studies hold the potential to save the eyesight of millions of glaucoma patients.”
The findings have been the culmination of nearly two decades of research with Lieberman’s close collaborator, University of Texas at Austin chemical engineering Professor Jennifer Maynard, whose group helped discover the two antibodies that responded to the mutation. Lieberman’s group then worked to understand how the antibodies functioned, determining the two that most successfully broke down the protein.
“This study builds on 10 years of work that explains how myocilin folds to how to break it down,” Lieberman said. “I am at a very fortunate place in my career where this fundamental research coalesces into what we could use clinically.”
Treatment Transformation
Lieberman hopes the antibodies can help treat glaucoma patients, particularly those with early onset glaucoma, often children. She now has a research collaboration with Rebecca Neustein, a physician at Emory University who treats these young patients.
“She doesn't have much hope to give her patients for curing glaucoma,” Lieberman said. “So she was very excited that we could do some genotyping and figure out who these antibodies can help.”
Lieberman’s research offers a clearer future for millions suffering from glaucoma and those at risk of developing the disease. By leveraging antibodies to target and break down malfunctioning myocilin, this discovery not only paves the way for new treatments for glaucoma but also opens doors for addressing other protein-aggregation diseases like Alzheimer’s, Parkinson’s, and even Type 2 diabetes.
Funding: National Institutes of Health
Animation by Raul Perez
For More Information Contact
Tess Malone, Senior Research Writer/Editor
tess.malone@gatech.edu